The aims of this Palliative Medicine subspecialist training programme are to ensure that the trainees have sufficient broad-based training and in-depth clinical exposure to function as consultants in a variety of care settings, so as to be able:
- To provide consultative and advisory service to physicians and surgeons in hospitals regarding the palliative care of their patients.
- To provide direct care to patients and families in a variety of care settings including hospital wards, clinics, and community settings (including at home, in inpatient hospices, palliative wards or nursing homes etc.)
- To be core members and even leaders of interdisciplinary palliative care teams and palliative care services.
- To be critical thinkers who are committed to continuous learning and professional development, whether as a learner or as a teacher.
- To advocate for access to quality palliative care for all who need it.
Rotations & Electives
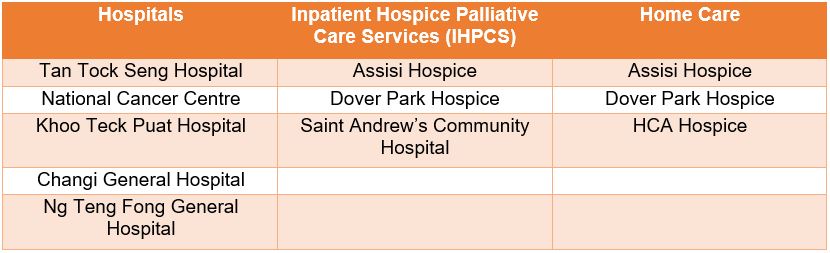
Palliative Medicine residents will be attached to Palliative care services in acute hospitals, inpatient hospice palliative care services (IHPCS) and hospice home care services. They will also get a chance to do electives of their choice in specialties such as Radiation Oncology, Medical Oncology, etc. For entrants with Master of Medicine in Family Medicine or have completed Family Medicine Residency, it is compulsory to do Medical Oncology as an elective.
/2)%20Rotations%20%26%20Electives%20-%20Updated.jpg)
Residents would be posted to the following accredited training sites for their training.